Heart Murmur
Page 1 of 1
 Heart Murmur
Heart Murmur
Aortic Stenosis
Crescendo-decrescendo systolic murmur that radiates to carotids. "pulsus parvus et tardus". Poor & delayed.
How does this show up on Step1? Patient with exertional SAD: syncope, angina, dyspnea. AS + any of the 3 SAD symptoms warrant aortic valve replacement.
↑ Anything that increases venous return/preload and heart volume, i.e. going from standing/sitting to lying down (recumbent), giving fluids, raising leg, squatting
↓ Anything that decreases venous return/preload and heart volume, i.e. standing up from recumbent, nitrates, diuretics, hand grip. Why hand grip? It raises SVR without affecting venous return. The increase in systemic vascular resistance decreases the trans-aortic valve pressure gradient, thereby diminishing the turbulent flow and intensity of the aortic stenosis murmur
No.1 cause in the elderly, (generally step1 rule of thumb >70 years old) is caused by calcific sclerosis "calcium hardening" of aortic valve
No.1 cause in the young (<70 years old) is bicuspid aortic valve
If it's young patient who recently IMMIGRATED to the US, think rheumatic fever, aortic stenosis (mitral stenosis most common, but can affect aortic valve)
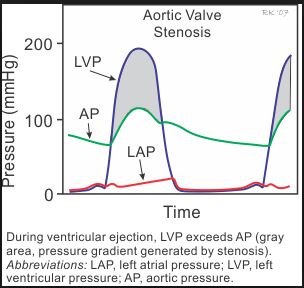
Image credit: CV Physiology
Aortic Regurgitation
Blowing or high-pitched diastolic decrescendo murmur.
Best heard how and where? With patient sitting up and leaning forward. Why? This position displaces the heart anteriorly to accentuate the faint diastolic regurgitant murmur. Ask patient to expire fully. Why? Expiration decreases lung volume, increases intrathoracic pressure which facilitates blood flow into the left ventricle, thereby increasing intra-chamber blood volume and therefore "increases left heart volume".
How does this show up on Step1? Usually in the sitting of aortic root dilation secondary to tertiary syphilis, bacterial endocarditis, Marfan syndrome. Patient will classically present with WIDENED pulse pressure. Why? The regurgitant jet causes less effective stroke volume, which puts increased demand on the ventricle to hypertrophy and eject more volume, thereby increasing the Systolic BP value. However, regurgitation also "robs" the arterial/arterioles of the diastolic pressure because less blood are in the arterial system during diastole, thereby decreasing this value. In other words, the systemic pressure during diastole drops precipitously as the blood flows from the aorta back through the incompetent aortic valve into the left ventricle. This increased heart pumping to meet demand with subsequent backflow causes "HEAD BOBBING, waterhammer pulse, bounding pulse, hyperdynamic precordium, ventricular heave/lift".
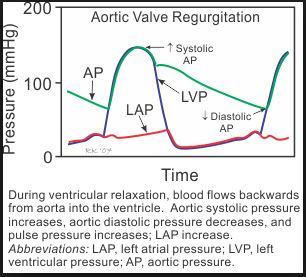
Image credit: CV Physiology
Mitral Stenosis
Late diastolic rumbling murmur. (Yes, it occurs after opening snap, but I hardly ever hear this on an exam. I just listen for a first S1 heart sound, pause, and then a faint diastolic rumble).
Where is it best heart? With patient in left lateral decubitus position (LLD). Why? This brings the left side of the heart more anteriorly.
How does this show up on Step1? In setting of IMMIGRANT, previous bacterial strep pharyngitis (either NOT treated or Inadequately treated without appropriate type and duration of antibiotics) resulting in rheumatic fever. Patient comes in saying, "doc I have hard time breathing or my voice changed, and recently noticed some pinkish tinge to my expectorated sputum", and usually an auscultation multimedia where you have to move your stethoscope cursor over the yellow circles.
1. Why difficulty breathing? MS impairs LV filling and cardiac output. Second, all that blood backs up into the left atrium and pulmonary vessels leading to interstitial edema and later pulmonary edema. Hence = "heart failure" dyspnea
2. Why voice change? Atrial dilation compressing recurrent laryngeal nerve which innervates All intrinsic laryngeal muscles except cricothyroid muscle (superior laryngeal nerve ***anatomy Step1)
3. Why pinkish sputum? Pulmonary edema also contributes to alveolar capillary leak and spilling of RBC leading to non-emergent hemoptysis
What FIRST AID teaches you: As the interval of S2 and OS (opening snap) shortens, the snap murmur intensity increases. This is because the more severely stenotic mitral valve also has concomittant taut chordae tendinae and the leaflet motion occurs sooner after S2. In fact, with Severe Mitral Stenosis, this entirely eliminates S1 altogether (wait but what about tricuspid valve? Its closure contributes less to the S1 heart sound than does mitral valve).
***Rheumatic Fever: It's a dysregulated "auto" immune reactivity to previously microbial infection that cross-reacts with similar antigenic epitopes on host cells. Commonly occurs during Group A Strep (beta-hemolytic) pharyngitis or less commonly, cellulitis. Therefore, Anti-microbials will not work as there are no bacterial. BUT, for rheumatic fever, the correct STEP1 response and the standard of care is still to give antibiotics to anyone with previously untreated Strep throat for prophylaxis against and therapeutic treatment for rheumatic symptoms. Abx include oral Amoxicillin, PCN G benzathine, PCN V (AHA Guidelines on Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute Streptococcal Pharyngitis)
1. When this "molecular mimicry" happens on cardiac myocytes, this is called Rheumatic Fever
2. When this "molecular mimicry" happens on glomerular cells, this is called Post-Strep GlomeruloNephritis (PSGN). Step1 caveat: While Antibiotic given at time of strep throat can prevent rheumatic fever, such treatment principle can NOT prevent PSGN. So, how do you treat PSGN? Watch for worsening edema and/or HTN for which you must restrict water, then give diuretics, then try ACEi or ARB. IV Nitroprusside for Malignant HTN. Dialysis for Uremia or symptomatic HyperKALEMIA. Steroids, Immunosuppression, and Plasmapheresis are NOT indicated. Remember when do you perform plasmapheresis? TTP-HUS
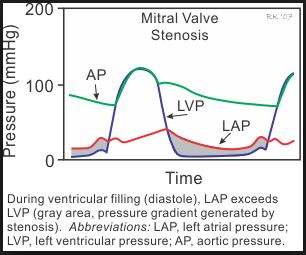
Image credit: CV Physiology
Mitral Regurgitation
Holosystolic "blowing" or "high-pitched" murmur that radiates to the cardiac apex or axilla.
How does this show up on STEP1?
1) Infective Endocarditis. How? Fragments of "infectious vegetation" aka bacteria + fibrin clot + debris can break off and travel to the heart, whereby they settle on any of the heart valves and cause valvular incompetence and regurgitation. Most commonly Mitral Valve > Tricuspid Valve. When tricuspid valve is involved, always think IV Drug Use with Staph colonization.
2) Post Myocardial Infarcation. How? Either anterior wall (V1-V4) or inferior wall (II, III, aVF) MI can disrupt either anterior or posterior mitral valve leaflet.
3) Worsening MVP. How? Severe prolapse can cause valvular incompetence.
4) Aortic Dissection. How? Dissection to aorta and rarely through entire atrium to mitral valve. Most commonly = aortic dissection ==> aortic regurgitation.
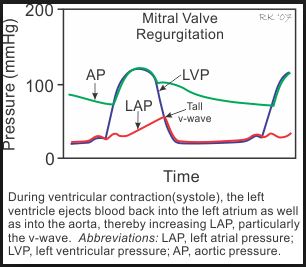
Image credit: CV Physiology
Hypertrophic Obstructive Cardiomyopathy (HOCM)
Similar to AS, also crescendo-decrescendo murmur. However, unlike AS, this murmur intensifies with maneuvers that "Shrink the heart" i.e. decrease venous return and preload (nitrates, diuretics, standing up, Valsalva).
How does this show up on STEP1? Young athlete with sudden cardiac death. They can ask:
1) What's the pathogenesis? Tissue biopsy will show myofibril disarray aka disorganized cardiac muscle fibers
2) What's the pathophysiology? Asymmetric ventricular and interventricular septal hypertrophy resulting in abnormal motion of the mitral valve leaflet against septum during systolic ventricular contraction, such that this narrows the ventricular outflow tract resulting in SAD (syncope, angina, dyspnea).
3) Why sudden death? No.1 cause is not because of the outflow obstruction, but likely due to the cardiac structural derangement, which leads to significantly heightened risk for arrythmia. And what arrhythmia kills? Ventricular Fibrillation. So what's no.1 cause of death in HOCM patients (and for that matter, all patients in general with Structural heart disease)? Arrhythmia = Vfib
Tricuspid Regurgitation/Stenosis
How does this show up on STEP1? Anytime tricuspid murmur is mentioned i.e. (either Right or Left Lower Sternal Border), or a murmur that accentuates/increases with INSPIRATION*** think of the following.
1) IV Drug Use
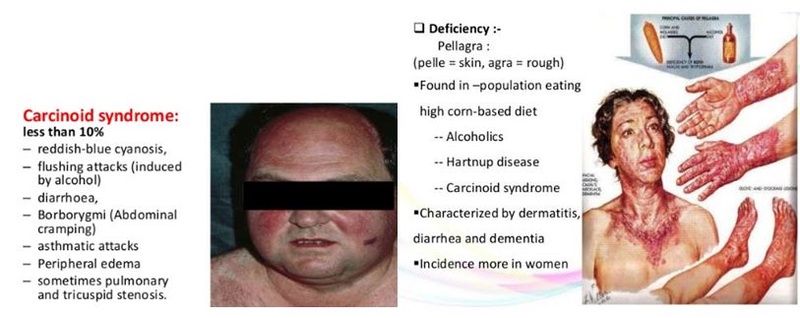
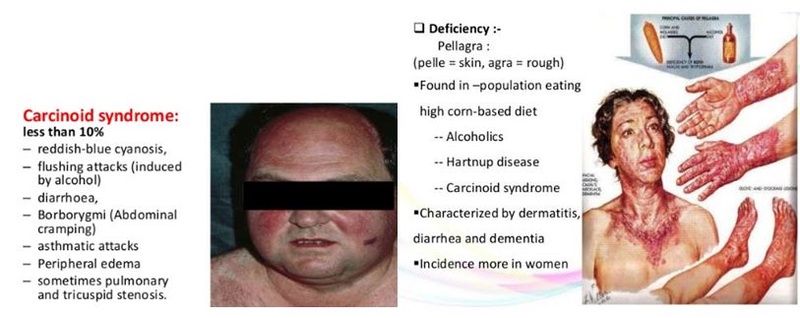
2) Carcinoid Syndrome: Remember your "-ing" diarrhea-ing, wheez-ing, flush-ing, tricuspid-ing. Carcinoid tumor most commonly arises in small bowel (ileum). However, carcinoid tumor in of itself does NOT cause carcinoid SYNDROME. Why not? They are relatively Asymptomatic until they metastasize to the liver, because the liver metabolize many of the metabolic toxins responsible for the "ing" symptoms. Nonetheless, once metastasis has occurred to the liver, these toxins bypass hepatic processing on route to the right heart and lung. Hence tricuspid murmur and wheezing. What's the serum or urine marker? 5HIAA. Why can carcinoid syndrome cause dermatitis, diarrhea, dementia of Pellagra (Niacin VitB3 deficiency)? serotonin and less tryptophan available for VitB3 synthesis. What's the treatment? Octreotide
So Carcinoid: ing-ing-ing-ing. Pellagra: D-D-D
***So why does Tricuspid murmur increase with INSPIRATION?
You INSPIRE into your right heart and you EXPIRE into your left heart. The lengthy explanation: Inspiration increases lung volume and decreases intrathoracic pressure which does two things 1)Increases venous return the right heart, thereby increasing right heart volume 2) "increases pulmonary vascular dilation, which holds blood in the pulmonary circulation, thereby decreasing blood return to left atrium and decreasing left heart volume. Together, the increase in right heart volume and slight decrease in left heart volume also sets up a physical anatomic discrepancy, whereby the septum deviates to the left, further restricting left ventricular volume. This ultimately causes decreased stroke volume during inspiration, only to be compensated by a physiologic increase in heart rate and contractility to meet tissue demand. Thus when you inspire, your heart beats faster.
Conversely, expiration does the opposite. Decreased intrathoracic pressure impedes venous return to the right heart, but favors pulmonary blood flow towards left atrium. That's why you expire into your left heart and slow down your heart rate that was previously accelerated by inspiration.
Final note: the septal deviation and reflexive tachycardia and transient drop in blood pressure is physiologic. Certain pathologies can exacerbate this deviation and subsequent tachycardia/hypotension. What is the condition called? Pulsus Paradoxus. What are the causes and why?
1) Cardiac Tamponade: Bleeding into the pericardial sac leads to severely impaired venous return to right side such that upon inspiration, the blood pressure drops precipitously and jugular venous pressures fail to decline (aka dilated jugular veins = Kussmaul sign). This is an emergency, warranting bedside-ultrasound (transthoracic echo) for diagnosis and urgent pericardiocentesis.
2) Severe Asthma/emphysema: With air-trapping and lung hyperinflation, this is like taking inspiration to the extreme. Imagine, super inflated lungs which decreases intra-thoracic pressure tremendously. This "BIG INSPIRATION" greatly increases your right heart volume at the expense of your left heart volume. Hence, you have an exaggerated septal deviation with subsequent fall in stroke volume and >20mmHg drop in systolic BP and pulsus paradoxus.
Ventricular Septal Defect (VSD)
Holosystolic murmur at right or left lower sternal border. Remember Tricuspid regurgitation also is a holosystolic murmur at RLSB or LLSB. So how do you tell the difference? VSD is not associated with IVDU or Carcinoid Syndrome and does NOT accentuate in intensity with inspiration.
The larger the ventricular defect, the quieter the murmur
Maneuvers that increase the heart volume makes the murmur louder, i.e. (squatting, giving fluids, lying down).
Maneuvers that increase the SVR makes the murmur louder, i.e. (hand grip, squatting, giving vasopressors such as epinephrine, dopamine)
Atrial Septal Defect (ASD)
This is a "weird murmur" in the sense that there's not really any specific pathognomonic features. Similar to VSD, it's holosystolic along the left sternal border. It can be associated with a pulmonic flow murmur. Why? The atrial defect allows blood from pulmonic side (left) to flow into systemic side (right) due to pressure gradient. The extra blood on right side causes a faint flow murmur across the pulmonic valve.
As with small VSD, small ASD if asymptomatic are best left alone. No treatment necessary.
S4
Extra heart sound right before S1, usually corresponding to the atrial exertion against increased resistance. Seen in setting of chronic systemic hypertension, aortic stenosis, etc. S4 in elderly is NORMAL (correlated with degree HTN), in the young is NOT normal.
On Step 1, associate S4 with decreased left ventricular compliance secondary to LV wall stiffening "concentric hypertrophy"
S3
Extra heart sound right after S2, usually corresponding to either increased reverberating blood in the cardiac chambers or increased volume tugging on tensed chordae tendinae. S3 is NORMAL in the young and pregnant, in the elderly is NOT normal. Either way, S3 on STEP1 means the following
1) Heart failure, dilated ventricles
2) Regurgitation murmurs, usually Mitral Regurg, dilated ventricles
3) Dilated cardiomyopathy (sarcoidosis, amyloidosis, hemochromatosis, alcohol, virus), dilated ventricles.
4) Can be observed in pregnancy and other hyperdynamic states like hyperthyroidism, Paget's disease, AV fistulas, anything with increased cardiac output.
Patent Ductus Arteriosus (PDA)
The classic Step1 or textbook description is "machine-gun murmur". Know what this sounds like on auscultation!!! This murmur can be heard pretty much on all the circles of the NBME auscultation interface, but most loudly at infraclavicular region.
1. What congenital disease in childhood/newborn? Rubella. and Prematurity
2. What's the treatment? Indomethacin. How? NSAID blocks prostaglanding synthesis, PGE1 which normally keeps the ductus patent during fetal development.
3. How does this show up on STEP1? Newborn with pink/rosy face and pink/rosy upper extremity but blue legs and feet. Or a teenager who exercises and then gets winded and blue feet. Why? Anatomically the ductus is just distal to the left subclavian artery such that any mixing of blood occurs distal to the ductus, affecting primarily the trunk and lower extremities.
4. Remember "bounding pulses", "head-bobbing", "hyperdynamic precordium", "ventricular heave/lift"? When you see these terms, think of two murmurs. Aortic regurgitation vs. PDA. Already explained how AR causes bounding pulses secondary to widened pulse pressure. So why does PDA cause bounding pulses? Again the phenomenon is due to some ejected blood flowing through a detour, whether that detour is back through an incompetent aortic valve or its through a patent ductus. The regurgitant volume does not contribute to diastolic pressure and this creates an exaggerated widened pressure difference between systole and diastole.
5. Minimal aorta to pulmonary artery shunting from a small PDA is usually clinically insignificant. However, a larger PDA with clinically evident shunting (dyspnea, cyanosis, exercise intolerance) can lead to left-sided volume overload, heart failure, pulmonary hypertension, and eventually Eisenmenger's syndrome.
6. STEP1 caveat. They love to test if you know how to differentiate PDA and aortic coarctation. Both present with exercise intolerance. However, aortic coarctation does not involve cyanosis. Rather, there's a systolic BP difference in upper and lower extremities. PAY ATTENTION to vitals. Alternatively, instead of presenting with differing BP in UE & LE, they can say that the legs have atrophic or thin skin with "mottling", coarse brittle hair, or weak non-palpable femoral, dorsalis pedis, posterior tibial pulses, or that the kid gets muscle cramps when running, all of which which indicates chronic arterial insufficiency. Aortic Coarctation is also associated with Turner Syndrome and bicuspid aortic valve. Classic Chest X-ray can show rib notching secondary to intercostal collateral circulation.
Maneuvers and their Effects
1. Inspiration: increases venous return to right heart, while decreasing pulmonary return to left heart. Increases "tricuspid" murmurs, useful in patients with IVDU, Carcinoid syndrome, infectious endocarditis of tricuspid valve
2. Hand Grip or any "contraction" or any drug that increases afterload, i.e. vasopressors epinephrine, dopamine: By contracting muscle, you're squeezing the muscle against arteries and arterioles, which raises the systemic vascular resistance and raises afterload. This increases intensity of most regurgitant and septal defect murmurs i.e. AR, MR, ASD, VSD. However, raising afterload decreases the aortic valvular gradient, thereby decreasing intensities of aortic stenosis and HOCM murmurs
3. Anything that "shrinks" the heart aka decreases preload, i.e. Valsalva, diuretics, standing up. Valsalva means to fight really hard against constipation, which entails tremendous abdominal muscle contraction, elevating intra-abdominal pressure, which translates into increasing intra-thoracic pressure. This increase in intra-thoracic pressure impedes venous return to the right heart. These maneuvers intensify HOCM murmur while diminishing AS murmur. MVP click occurs earlier. Why? "Smaller heart" less room for mitral valve leaflet to coapt and chordae tendinae to reverberate.
4. Rapid Squatting. Unlike hand grip, rapid squatting not only increases systemic vascular resistance (squatting squeezes your leg muscles and compress against arterioles) but also increases your venous return because it brings the rest of your lower extremity circulation closer to your heart, lowering the pressure gradient necessary to overcome gravity. This is exact opposite to Valsalva. So Squatting intensifies AS while quiets HOCM.
Sample Questions:
1. 71 year old man comes to his primary care physician complaining of increasing frequency of shortness of breath walking across the parking lot to and from his car when shopping with his wife. He sleeps with 3 pillows at night. Physical exam of patient sitting upright and leaning forward reveals a faint diastolic murmur heard at full expiration. What is another associated symptom of this condition?
A. Splinter Hemorrhages
B. Hoarseness
C. Hyperdynamic precordium
D. Pharyngitis
E. Flushing
Answer: C. Hyperdynamic precordium. One-liner summary: elderly p/w exertional dyspnea, nocturnal orthopnea, AR murmur.
2. Patient presents with fatigue, exertional dyspnea, and difficulty lying flat. Upon ausultation of the murmur, it is diastolic rumble heard best when patient is placed in left lateral decubitus position. What murmur is it?
A. Aortic Stenosis
B. Aortic Regurgitation
C. Mitral Stenosis
D. Mitral Regurgitation
E. Tricuspid Stenosis
F. Tricuspid Regurgitation
Answer: C. Mitral Stenosis.
3. What maneuver can intensify HOCM and make MVP click occur earlier in systole?
A. Hand Grip
B. Feet Grip
C. Squat
D. Standing from recumbent position
E. Recumbent position from standing
Answer: D. Standing from recumbent position. Also: Valsalva.
4. 57 year old man comes in complaining of crushing chest pain radiating to his jaw, diaphoresis, and dyspnea. Subsequent work-up with CBC, BMP, EKG, serial troponins, BNP reveal infarction of heart tissue. Patient is rushed to the interventional cardiology suite with emergent percutaneous coronary intervention. Patient is stabilized. Two days later, patient presents with sudden onset shortness of breath. On physical exam, a holosystolic blowing murmur is best heard at the apex radiating to the axilla. Which of the following marker is the best predictor of this murmur severity? (revised from Medbullets)
A. Presence of audible S3
B. Presence of audible S4
C. Enhancement with hand grip
D. Enhancement with expiration
E. Enhancement with inspiration
Answer: A. Presence of audible S3. Why? In you mind, anytime a new holosystolic murmur arise a few days after an acute MI, always think Mitral Regurgitation. Now, the question asks for what clinical marker predicts how severe is the MR, or how severe is the turbulent blood flow across the incompetent mitral valve. This murmur depends on 2 things. 1) valve function 2) blood volume which when increased contributes to turbulence and intensifies murmur. S3 is a good correlator of left ventricular volume. Hence, you see S3 in cases of heart failure, infiltrative dilated cardiomyopathy, and in mitral regurgitation.
5. A 37-year-old woman presents to clinic for routine checkup. She has no complaints with the exception of occasional "shortness of breath." Auscultation reveals "snap"-like sound after S2, followed by a rumbling murmur best heard at the cardiac apex. A history of which of the following are you most likely to elicit upon further questioning of this patient? (Medbullets revision)
A. Family history of aortic valve replacement at young age
B. Hyperflexibility, poor vision, spontaneous pneumothoraces
C. Systolic click on auscultation
D. Multiple episodes of untreated streptococcal pharyngitis
E. Cutaneous flushing, diarrhea, bronchospasm, murmur intensifies with inspiration
Answer: D. Multiple episodes of untreated streptococcal pharyngitis
A. Bicuspid aortic valve --> early aortic stenosis
B. Marfan syndrome --> aortic root dilatation = aortic regurgitation
C. Mitral Valve Prolapse
E. Carcinoid syndrome
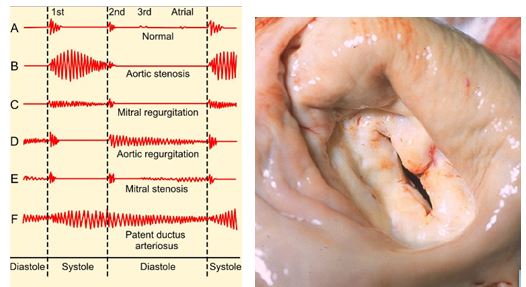
STEP1 Peril1. Stenotic valves caused by rheumatic fever involve fusion of their commissures. Normal calcific stenosis do NOT involve such fusion. See above right image: Notice that in addition to valvular lumen narrowing, there's fusion of the valve leaflets at their commissures, or where two leaflets meet at either end.
STEP1 Peril2. While you typically associated Rheumatic fever with Mitral Stenosis (diastolic rumbling murmur at apex), it can also cause MR (holosystolic blowing murmur at apex) or AS (radiating crescendo-decrescendo murmur to carotids) or AR (diastolic rumbling murmur at upper sternal border, bounding pusles)
6. What's the best diagnostic tool for assessing new murmurs?
Answer: Echocardiogram. Any DIASTOLIC, grade 3 or higher, murmur that intensify with Valsalva must be evaluated with echocardiogram.
7. A 38-year-old homeless man presents to local community clinic complaining of fatigue and paroxysmal fluctuating fevers for three days. Cardiac exam reveals a holosystolic murmur over the left lower sternal border that increases on inspiration. Exam of his forearm reveals the following.

What's the most likely diagnosis?
A. Cellulitis
B. Bacterial Endocarditis
C. Rheumatic Fever
D. Mycobacterium Tuberculosis
E. Malaria
Answer: B. Bacterial Endocarditis. Image shows needle track marks of an IV drug user. Murmur is tricuspid regurgitation secondary to infective endocarditis vegetation on tricuspid valve.
Crescendo-decrescendo systolic murmur that radiates to carotids. "pulsus parvus et tardus". Poor & delayed.
How does this show up on Step1? Patient with exertional SAD: syncope, angina, dyspnea. AS + any of the 3 SAD symptoms warrant aortic valve replacement.
↑ Anything that increases venous return/preload and heart volume, i.e. going from standing/sitting to lying down (recumbent), giving fluids, raising leg, squatting
↓ Anything that decreases venous return/preload and heart volume, i.e. standing up from recumbent, nitrates, diuretics, hand grip. Why hand grip? It raises SVR without affecting venous return. The increase in systemic vascular resistance decreases the trans-aortic valve pressure gradient, thereby diminishing the turbulent flow and intensity of the aortic stenosis murmur
No.1 cause in the elderly, (generally step1 rule of thumb >70 years old) is caused by calcific sclerosis "calcium hardening" of aortic valve
No.1 cause in the young (<70 years old) is bicuspid aortic valve
If it's young patient who recently IMMIGRATED to the US, think rheumatic fever, aortic stenosis (mitral stenosis most common, but can affect aortic valve)
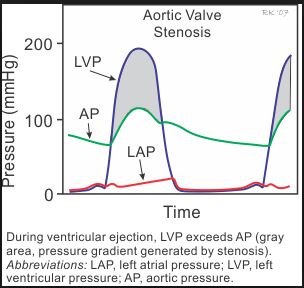
Image credit: CV Physiology
Aortic Regurgitation
Blowing or high-pitched diastolic decrescendo murmur.
Best heard how and where? With patient sitting up and leaning forward. Why? This position displaces the heart anteriorly to accentuate the faint diastolic regurgitant murmur. Ask patient to expire fully. Why? Expiration decreases lung volume, increases intrathoracic pressure which facilitates blood flow into the left ventricle, thereby increasing intra-chamber blood volume and therefore "increases left heart volume".
How does this show up on Step1? Usually in the sitting of aortic root dilation secondary to tertiary syphilis, bacterial endocarditis, Marfan syndrome. Patient will classically present with WIDENED pulse pressure. Why? The regurgitant jet causes less effective stroke volume, which puts increased demand on the ventricle to hypertrophy and eject more volume, thereby increasing the Systolic BP value. However, regurgitation also "robs" the arterial/arterioles of the diastolic pressure because less blood are in the arterial system during diastole, thereby decreasing this value. In other words, the systemic pressure during diastole drops precipitously as the blood flows from the aorta back through the incompetent aortic valve into the left ventricle. This increased heart pumping to meet demand with subsequent backflow causes "HEAD BOBBING, waterhammer pulse, bounding pulse, hyperdynamic precordium, ventricular heave/lift".
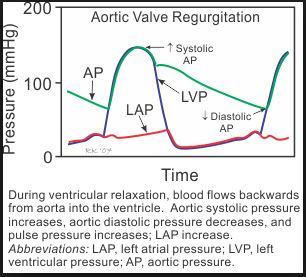
Image credit: CV Physiology
Mitral Stenosis
Late diastolic rumbling murmur. (Yes, it occurs after opening snap, but I hardly ever hear this on an exam. I just listen for a first S1 heart sound, pause, and then a faint diastolic rumble).
Where is it best heart? With patient in left lateral decubitus position (LLD). Why? This brings the left side of the heart more anteriorly.
How does this show up on Step1? In setting of IMMIGRANT, previous bacterial strep pharyngitis (either NOT treated or Inadequately treated without appropriate type and duration of antibiotics) resulting in rheumatic fever. Patient comes in saying, "doc I have hard time breathing or my voice changed, and recently noticed some pinkish tinge to my expectorated sputum", and usually an auscultation multimedia where you have to move your stethoscope cursor over the yellow circles.
1. Why difficulty breathing? MS impairs LV filling and cardiac output. Second, all that blood backs up into the left atrium and pulmonary vessels leading to interstitial edema and later pulmonary edema. Hence = "heart failure" dyspnea
2. Why voice change? Atrial dilation compressing recurrent laryngeal nerve which innervates All intrinsic laryngeal muscles except cricothyroid muscle (superior laryngeal nerve ***anatomy Step1)
3. Why pinkish sputum? Pulmonary edema also contributes to alveolar capillary leak and spilling of RBC leading to non-emergent hemoptysis
What FIRST AID teaches you: As the interval of S2 and OS (opening snap) shortens, the snap murmur intensity increases. This is because the more severely stenotic mitral valve also has concomittant taut chordae tendinae and the leaflet motion occurs sooner after S2. In fact, with Severe Mitral Stenosis, this entirely eliminates S1 altogether (wait but what about tricuspid valve? Its closure contributes less to the S1 heart sound than does mitral valve).
***Rheumatic Fever: It's a dysregulated "auto" immune reactivity to previously microbial infection that cross-reacts with similar antigenic epitopes on host cells. Commonly occurs during Group A Strep (beta-hemolytic) pharyngitis or less commonly, cellulitis. Therefore, Anti-microbials will not work as there are no bacterial. BUT, for rheumatic fever, the correct STEP1 response and the standard of care is still to give antibiotics to anyone with previously untreated Strep throat for prophylaxis against and therapeutic treatment for rheumatic symptoms. Abx include oral Amoxicillin, PCN G benzathine, PCN V (AHA Guidelines on Prevention of Rheumatic Fever and Diagnosis and Treatment of Acute Streptococcal Pharyngitis)
1. When this "molecular mimicry" happens on cardiac myocytes, this is called Rheumatic Fever
2. When this "molecular mimicry" happens on glomerular cells, this is called Post-Strep GlomeruloNephritis (PSGN). Step1 caveat: While Antibiotic given at time of strep throat can prevent rheumatic fever, such treatment principle can NOT prevent PSGN. So, how do you treat PSGN? Watch for worsening edema and/or HTN for which you must restrict water, then give diuretics, then try ACEi or ARB. IV Nitroprusside for Malignant HTN. Dialysis for Uremia or symptomatic HyperKALEMIA. Steroids, Immunosuppression, and Plasmapheresis are NOT indicated. Remember when do you perform plasmapheresis? TTP-HUS
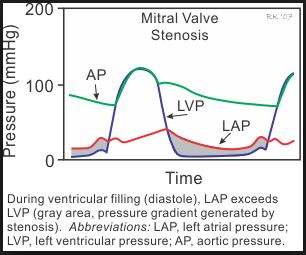
Image credit: CV Physiology
Mitral Regurgitation
Holosystolic "blowing" or "high-pitched" murmur that radiates to the cardiac apex or axilla.
How does this show up on STEP1?
1) Infective Endocarditis. How? Fragments of "infectious vegetation" aka bacteria + fibrin clot + debris can break off and travel to the heart, whereby they settle on any of the heart valves and cause valvular incompetence and regurgitation. Most commonly Mitral Valve > Tricuspid Valve. When tricuspid valve is involved, always think IV Drug Use with Staph colonization.
2) Post Myocardial Infarcation. How? Either anterior wall (V1-V4) or inferior wall (II, III, aVF) MI can disrupt either anterior or posterior mitral valve leaflet.
3) Worsening MVP. How? Severe prolapse can cause valvular incompetence.
4) Aortic Dissection. How? Dissection to aorta and rarely through entire atrium to mitral valve. Most commonly = aortic dissection ==> aortic regurgitation.
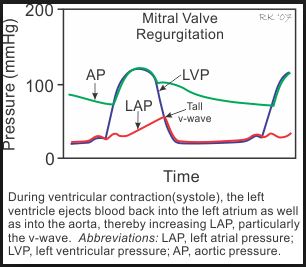
Image credit: CV Physiology
Hypertrophic Obstructive Cardiomyopathy (HOCM)
Similar to AS, also crescendo-decrescendo murmur. However, unlike AS, this murmur intensifies with maneuvers that "Shrink the heart" i.e. decrease venous return and preload (nitrates, diuretics, standing up, Valsalva).
How does this show up on STEP1? Young athlete with sudden cardiac death. They can ask:
1) What's the pathogenesis? Tissue biopsy will show myofibril disarray aka disorganized cardiac muscle fibers
2) What's the pathophysiology? Asymmetric ventricular and interventricular septal hypertrophy resulting in abnormal motion of the mitral valve leaflet against septum during systolic ventricular contraction, such that this narrows the ventricular outflow tract resulting in SAD (syncope, angina, dyspnea).
3) Why sudden death? No.1 cause is not because of the outflow obstruction, but likely due to the cardiac structural derangement, which leads to significantly heightened risk for arrythmia. And what arrhythmia kills? Ventricular Fibrillation. So what's no.1 cause of death in HOCM patients (and for that matter, all patients in general with Structural heart disease)? Arrhythmia = Vfib
Tricuspid Regurgitation/Stenosis
How does this show up on STEP1? Anytime tricuspid murmur is mentioned i.e. (either Right or Left Lower Sternal Border), or a murmur that accentuates/increases with INSPIRATION*** think of the following.
1) IV Drug Use
2) Carcinoid Syndrome: Remember your "-ing" diarrhea-ing, wheez-ing, flush-ing, tricuspid-ing. Carcinoid tumor most commonly arises in small bowel (ileum). However, carcinoid tumor in of itself does NOT cause carcinoid SYNDROME. Why not? They are relatively Asymptomatic until they metastasize to the liver, because the liver metabolize many of the metabolic toxins responsible for the "ing" symptoms. Nonetheless, once metastasis has occurred to the liver, these toxins bypass hepatic processing on route to the right heart and lung. Hence tricuspid murmur and wheezing. What's the serum or urine marker? 5HIAA. Why can carcinoid syndrome cause dermatitis, diarrhea, dementia of Pellagra (Niacin VitB3 deficiency)? serotonin and less tryptophan available for VitB3 synthesis. What's the treatment? Octreotide
So Carcinoid: ing-ing-ing-ing. Pellagra: D-D-D
***So why does Tricuspid murmur increase with INSPIRATION?
You INSPIRE into your right heart and you EXPIRE into your left heart. The lengthy explanation: Inspiration increases lung volume and decreases intrathoracic pressure which does two things 1)Increases venous return the right heart, thereby increasing right heart volume 2) "increases pulmonary vascular dilation, which holds blood in the pulmonary circulation, thereby decreasing blood return to left atrium and decreasing left heart volume. Together, the increase in right heart volume and slight decrease in left heart volume also sets up a physical anatomic discrepancy, whereby the septum deviates to the left, further restricting left ventricular volume. This ultimately causes decreased stroke volume during inspiration, only to be compensated by a physiologic increase in heart rate and contractility to meet tissue demand. Thus when you inspire, your heart beats faster.
Conversely, expiration does the opposite. Decreased intrathoracic pressure impedes venous return to the right heart, but favors pulmonary blood flow towards left atrium. That's why you expire into your left heart and slow down your heart rate that was previously accelerated by inspiration.
Final note: the septal deviation and reflexive tachycardia and transient drop in blood pressure is physiologic. Certain pathologies can exacerbate this deviation and subsequent tachycardia/hypotension. What is the condition called? Pulsus Paradoxus. What are the causes and why?
1) Cardiac Tamponade: Bleeding into the pericardial sac leads to severely impaired venous return to right side such that upon inspiration, the blood pressure drops precipitously and jugular venous pressures fail to decline (aka dilated jugular veins = Kussmaul sign). This is an emergency, warranting bedside-ultrasound (transthoracic echo) for diagnosis and urgent pericardiocentesis.
2) Severe Asthma/emphysema: With air-trapping and lung hyperinflation, this is like taking inspiration to the extreme. Imagine, super inflated lungs which decreases intra-thoracic pressure tremendously. This "BIG INSPIRATION" greatly increases your right heart volume at the expense of your left heart volume. Hence, you have an exaggerated septal deviation with subsequent fall in stroke volume and >20mmHg drop in systolic BP and pulsus paradoxus.
Ventricular Septal Defect (VSD)
Holosystolic murmur at right or left lower sternal border. Remember Tricuspid regurgitation also is a holosystolic murmur at RLSB or LLSB. So how do you tell the difference? VSD is not associated with IVDU or Carcinoid Syndrome and does NOT accentuate in intensity with inspiration.
The larger the ventricular defect, the quieter the murmur
Maneuvers that increase the heart volume makes the murmur louder, i.e. (squatting, giving fluids, lying down).
Maneuvers that increase the SVR makes the murmur louder, i.e. (hand grip, squatting, giving vasopressors such as epinephrine, dopamine)
Atrial Septal Defect (ASD)
This is a "weird murmur" in the sense that there's not really any specific pathognomonic features. Similar to VSD, it's holosystolic along the left sternal border. It can be associated with a pulmonic flow murmur. Why? The atrial defect allows blood from pulmonic side (left) to flow into systemic side (right) due to pressure gradient. The extra blood on right side causes a faint flow murmur across the pulmonic valve.
As with small VSD, small ASD if asymptomatic are best left alone. No treatment necessary.
S4
Extra heart sound right before S1, usually corresponding to the atrial exertion against increased resistance. Seen in setting of chronic systemic hypertension, aortic stenosis, etc. S4 in elderly is NORMAL (correlated with degree HTN), in the young is NOT normal.
On Step 1, associate S4 with decreased left ventricular compliance secondary to LV wall stiffening "concentric hypertrophy"
S3
Extra heart sound right after S2, usually corresponding to either increased reverberating blood in the cardiac chambers or increased volume tugging on tensed chordae tendinae. S3 is NORMAL in the young and pregnant, in the elderly is NOT normal. Either way, S3 on STEP1 means the following
1) Heart failure, dilated ventricles
2) Regurgitation murmurs, usually Mitral Regurg, dilated ventricles
3) Dilated cardiomyopathy (sarcoidosis, amyloidosis, hemochromatosis, alcohol, virus), dilated ventricles.
4) Can be observed in pregnancy and other hyperdynamic states like hyperthyroidism, Paget's disease, AV fistulas, anything with increased cardiac output.
Patent Ductus Arteriosus (PDA)
The classic Step1 or textbook description is "machine-gun murmur". Know what this sounds like on auscultation!!! This murmur can be heard pretty much on all the circles of the NBME auscultation interface, but most loudly at infraclavicular region.
1. What congenital disease in childhood/newborn? Rubella. and Prematurity
2. What's the treatment? Indomethacin. How? NSAID blocks prostaglanding synthesis, PGE1 which normally keeps the ductus patent during fetal development.
3. How does this show up on STEP1? Newborn with pink/rosy face and pink/rosy upper extremity but blue legs and feet. Or a teenager who exercises and then gets winded and blue feet. Why? Anatomically the ductus is just distal to the left subclavian artery such that any mixing of blood occurs distal to the ductus, affecting primarily the trunk and lower extremities.
4. Remember "bounding pulses", "head-bobbing", "hyperdynamic precordium", "ventricular heave/lift"? When you see these terms, think of two murmurs. Aortic regurgitation vs. PDA. Already explained how AR causes bounding pulses secondary to widened pulse pressure. So why does PDA cause bounding pulses? Again the phenomenon is due to some ejected blood flowing through a detour, whether that detour is back through an incompetent aortic valve or its through a patent ductus. The regurgitant volume does not contribute to diastolic pressure and this creates an exaggerated widened pressure difference between systole and diastole.
5. Minimal aorta to pulmonary artery shunting from a small PDA is usually clinically insignificant. However, a larger PDA with clinically evident shunting (dyspnea, cyanosis, exercise intolerance) can lead to left-sided volume overload, heart failure, pulmonary hypertension, and eventually Eisenmenger's syndrome.
6. STEP1 caveat. They love to test if you know how to differentiate PDA and aortic coarctation. Both present with exercise intolerance. However, aortic coarctation does not involve cyanosis. Rather, there's a systolic BP difference in upper and lower extremities. PAY ATTENTION to vitals. Alternatively, instead of presenting with differing BP in UE & LE, they can say that the legs have atrophic or thin skin with "mottling", coarse brittle hair, or weak non-palpable femoral, dorsalis pedis, posterior tibial pulses, or that the kid gets muscle cramps when running, all of which which indicates chronic arterial insufficiency. Aortic Coarctation is also associated with Turner Syndrome and bicuspid aortic valve. Classic Chest X-ray can show rib notching secondary to intercostal collateral circulation.
Maneuvers and their Effects
1. Inspiration: increases venous return to right heart, while decreasing pulmonary return to left heart. Increases "tricuspid" murmurs, useful in patients with IVDU, Carcinoid syndrome, infectious endocarditis of tricuspid valve
2. Hand Grip or any "contraction" or any drug that increases afterload, i.e. vasopressors epinephrine, dopamine: By contracting muscle, you're squeezing the muscle against arteries and arterioles, which raises the systemic vascular resistance and raises afterload. This increases intensity of most regurgitant and septal defect murmurs i.e. AR, MR, ASD, VSD. However, raising afterload decreases the aortic valvular gradient, thereby decreasing intensities of aortic stenosis and HOCM murmurs
3. Anything that "shrinks" the heart aka decreases preload, i.e. Valsalva, diuretics, standing up. Valsalva means to fight really hard against constipation, which entails tremendous abdominal muscle contraction, elevating intra-abdominal pressure, which translates into increasing intra-thoracic pressure. This increase in intra-thoracic pressure impedes venous return to the right heart. These maneuvers intensify HOCM murmur while diminishing AS murmur. MVP click occurs earlier. Why? "Smaller heart" less room for mitral valve leaflet to coapt and chordae tendinae to reverberate.
4. Rapid Squatting. Unlike hand grip, rapid squatting not only increases systemic vascular resistance (squatting squeezes your leg muscles and compress against arterioles) but also increases your venous return because it brings the rest of your lower extremity circulation closer to your heart, lowering the pressure gradient necessary to overcome gravity. This is exact opposite to Valsalva. So Squatting intensifies AS while quiets HOCM.
Sample Questions:
1. 71 year old man comes to his primary care physician complaining of increasing frequency of shortness of breath walking across the parking lot to and from his car when shopping with his wife. He sleeps with 3 pillows at night. Physical exam of patient sitting upright and leaning forward reveals a faint diastolic murmur heard at full expiration. What is another associated symptom of this condition?
A. Splinter Hemorrhages
B. Hoarseness
C. Hyperdynamic precordium
D. Pharyngitis
E. Flushing
Answer: C. Hyperdynamic precordium. One-liner summary: elderly p/w exertional dyspnea, nocturnal orthopnea, AR murmur.
2. Patient presents with fatigue, exertional dyspnea, and difficulty lying flat. Upon ausultation of the murmur, it is diastolic rumble heard best when patient is placed in left lateral decubitus position. What murmur is it?
A. Aortic Stenosis
B. Aortic Regurgitation
C. Mitral Stenosis
D. Mitral Regurgitation
E. Tricuspid Stenosis
F. Tricuspid Regurgitation
Answer: C. Mitral Stenosis.
3. What maneuver can intensify HOCM and make MVP click occur earlier in systole?
A. Hand Grip
B. Feet Grip
C. Squat
D. Standing from recumbent position
E. Recumbent position from standing
Answer: D. Standing from recumbent position. Also: Valsalva.
4. 57 year old man comes in complaining of crushing chest pain radiating to his jaw, diaphoresis, and dyspnea. Subsequent work-up with CBC, BMP, EKG, serial troponins, BNP reveal infarction of heart tissue. Patient is rushed to the interventional cardiology suite with emergent percutaneous coronary intervention. Patient is stabilized. Two days later, patient presents with sudden onset shortness of breath. On physical exam, a holosystolic blowing murmur is best heard at the apex radiating to the axilla. Which of the following marker is the best predictor of this murmur severity? (revised from Medbullets)
A. Presence of audible S3
B. Presence of audible S4
C. Enhancement with hand grip
D. Enhancement with expiration
E. Enhancement with inspiration
Answer: A. Presence of audible S3. Why? In you mind, anytime a new holosystolic murmur arise a few days after an acute MI, always think Mitral Regurgitation. Now, the question asks for what clinical marker predicts how severe is the MR, or how severe is the turbulent blood flow across the incompetent mitral valve. This murmur depends on 2 things. 1) valve function 2) blood volume which when increased contributes to turbulence and intensifies murmur. S3 is a good correlator of left ventricular volume. Hence, you see S3 in cases of heart failure, infiltrative dilated cardiomyopathy, and in mitral regurgitation.
5. A 37-year-old woman presents to clinic for routine checkup. She has no complaints with the exception of occasional "shortness of breath." Auscultation reveals "snap"-like sound after S2, followed by a rumbling murmur best heard at the cardiac apex. A history of which of the following are you most likely to elicit upon further questioning of this patient? (Medbullets revision)
A. Family history of aortic valve replacement at young age
B. Hyperflexibility, poor vision, spontaneous pneumothoraces
C. Systolic click on auscultation
D. Multiple episodes of untreated streptococcal pharyngitis
E. Cutaneous flushing, diarrhea, bronchospasm, murmur intensifies with inspiration
Answer: D. Multiple episodes of untreated streptococcal pharyngitis
A. Bicuspid aortic valve --> early aortic stenosis
B. Marfan syndrome --> aortic root dilatation = aortic regurgitation
C. Mitral Valve Prolapse
E. Carcinoid syndrome
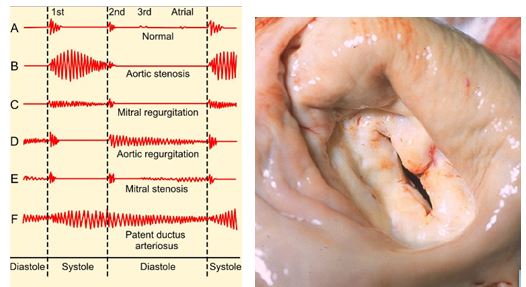
STEP1 Peril1. Stenotic valves caused by rheumatic fever involve fusion of their commissures. Normal calcific stenosis do NOT involve such fusion. See above right image: Notice that in addition to valvular lumen narrowing, there's fusion of the valve leaflets at their commissures, or where two leaflets meet at either end.
STEP1 Peril2. While you typically associated Rheumatic fever with Mitral Stenosis (diastolic rumbling murmur at apex), it can also cause MR (holosystolic blowing murmur at apex) or AS (radiating crescendo-decrescendo murmur to carotids) or AR (diastolic rumbling murmur at upper sternal border, bounding pusles)
6. What's the best diagnostic tool for assessing new murmurs?
Answer: Echocardiogram. Any DIASTOLIC, grade 3 or higher, murmur that intensify with Valsalva must be evaluated with echocardiogram.
7. A 38-year-old homeless man presents to local community clinic complaining of fatigue and paroxysmal fluctuating fevers for three days. Cardiac exam reveals a holosystolic murmur over the left lower sternal border that increases on inspiration. Exam of his forearm reveals the following.

What's the most likely diagnosis?
A. Cellulitis
B. Bacterial Endocarditis
C. Rheumatic Fever
D. Mycobacterium Tuberculosis
E. Malaria
Answer: B. Bacterial Endocarditis. Image shows needle track marks of an IV drug user. Murmur is tricuspid regurgitation secondary to infective endocarditis vegetation on tricuspid valve.
Page 1 of 1
Permissions in this forum:
You cannot reply to topics in this forum